View the full Article on:
Addimmune
Author: Addimmune Staff

Gene therapy has emerged as a logical approach for treating lifelong conditions, be it inherited disorders or persistent viral infections.
When faced with a lifelong condition, would you rather take a lifetime of pills, or would you prefer living with modified versions of your own cells that can effectively manage the disease for you? Thanks to the remarkable advancements in genetic technologies, long-lasting gene and cell therapies are becoming increasingly prevalent. On April 28th, 2023, The Washington Post published an article titled “A New Era for Treating Sickle Cell Disease Could Spark a Health-Care Revolution,” which showcased the struggle and triumph of Jimi Olaghere. Jimi’s battle with sickle cell took a transformative turn when he underwent gene therapy which re-educated his cells and caused a significant improvement in his condition.
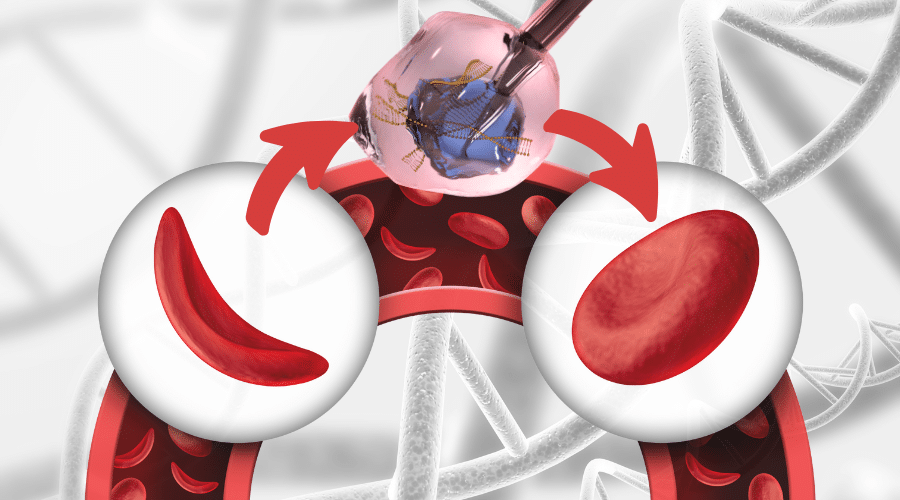
Briefly, sickle cell disease is an inherited condition which affects the function of red blood cells, which are important for the transportation of oxygen in the body. Normally, red blood cells are flexible and rounded so they fit through blood vessels, but individuals with sickle cell disease produce red blood cells which are rigid and sickle-shaped, which impedes blood flow and causes a cascade of symptoms. To address this genetic disorder, researchers have recently advanced a CRISPR/Cas9 based gene therapy into clinical trials aimed at functionally curing sickle cell disease. For Jimi Olaghere, the dramatic improvement in quality of life before and after therapy not only highlights the personal impact that genetic medicine can have, but also showcases the technological progress of these life -altering interventions. We are now squarely within the era of gene and cell therapy, and by understanding how scientists are editing blood cells, we can catch a glimpse of the future of genetic medicine.
How exactly do you edit someone’s blood cells?
Hematopoietic Stem Cells (HSCs) represent the essence of “lifeblood” as they possess the ability to divide and differentiate into various types of blood cells. Being the central hub in blood cell production and a self-renewing stem cell population, they present an attractive target for gene therapists. Modifying HSCs serves a dual purpose:
- When these stem cells replicate to create new stem cells, they establish a continuous source of the therapeutic genetic code.
- When the stem cells divide to form differentiated cell types, the resulting differentiated cells carry the therapeutic gene, allowing them to correct the disease.
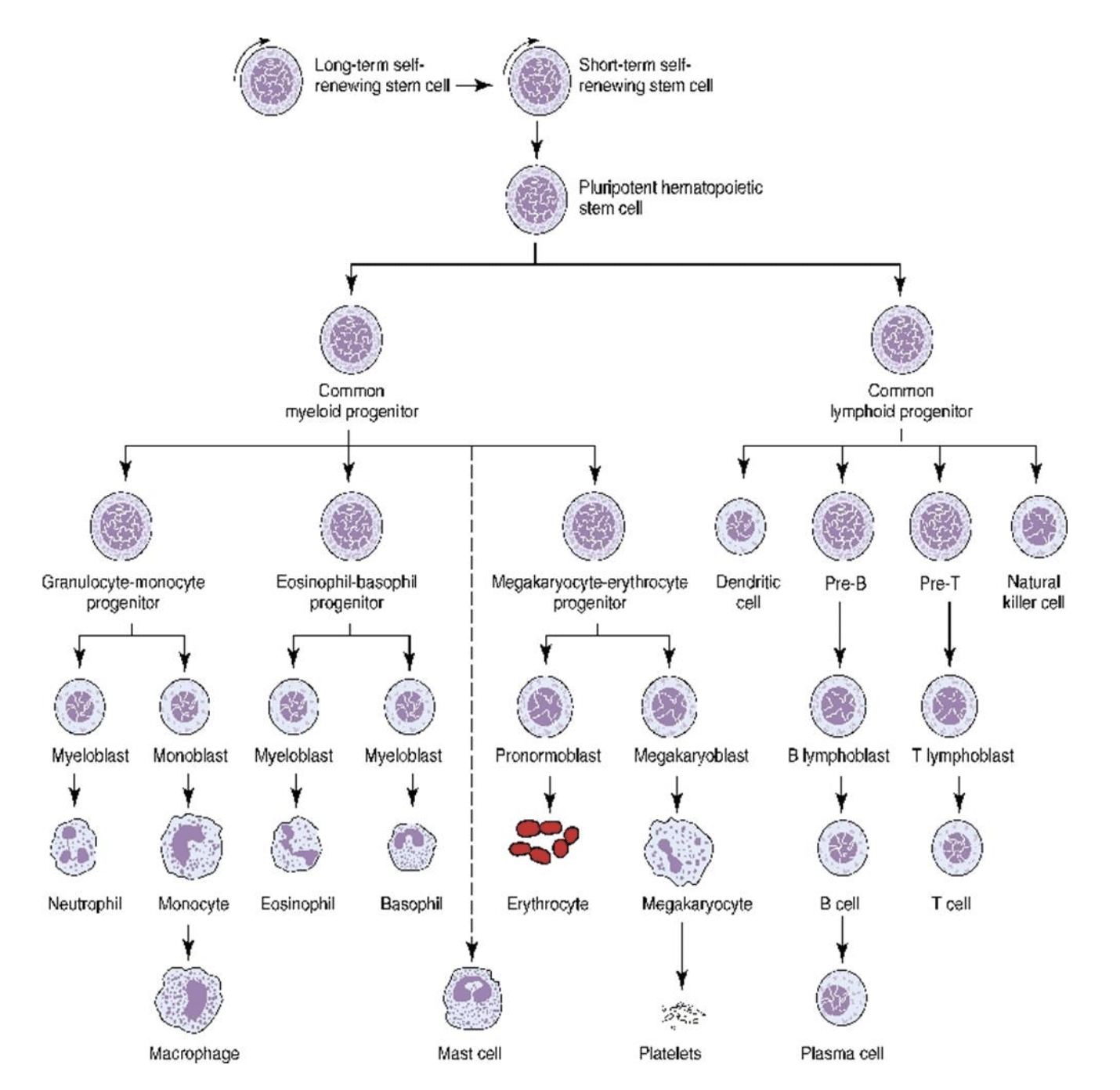
Figure 1: Hematopoiesis is the process of creating the various cell types of the blood from Hematopoietic Stem Cells (HSCs). Photo credit to Richard C. Meagher
To develop a gene therapy that ameliorates blood disorders like sickle cell, the next step is to select the appropriate tool for modifying the HSCs (or other stem-like cell populations) that will carry the gene therapy. Various tools are available today, ranging from old school Zinc Finger Nucleases (ZFNs) to more recent innovations like viral vectors and engineered CRISPR/Cas9 systems. By carefully selecting the right tool to modify the specific gene in the target cell, it becomes possible to create cells with the potential to effectively manage the disease throughout a person’s lifetime.
In the case of Jimi Olaghere’s sickle cell treatment, doctors extracted his HSCs, used a CRISPR/Cas9 system to target and edit the BCL11A gene, a negative regulator of fetal hemoglobin, and then reintroduced these near-identical cells back into his body. Under normal circumstances, adults do not produce fetal hemoglobin any more, but since researchers found that fetal hemoglobin was able to ameliorate sickle cell disease in mice, producing fetal hemoglobin seemed like a promising intervention. Jimi states in the article:
“I had lived 35 years with this disease that sometimes I consider a companion, and out of nowhere I could tell it had gone – or was in the process of leaving. We were enmeshed together, and I could feel it detangling.”
What other blood disorders can we use gene therapy for?
Blood-related conditions have become a focal point in gene and cell therapy research. With approved treatments for Hemophilia A, Hemophilia B, and multiple CAR-T therapeutics, the significance of gene therapy for blood cells cannot be underestimated. Here are a few reasons why blood cells are excellent targets:
- Blood cells are readily accessible compared to neurons or complex organ structures.
- Designing and testing a gene therapy for blood cells can be performed on cells outside the body, providing valuable insights into their performance within the body. This allows for data collection without necessarily requiring a human trial since the modified cells are not re-introduced into the patient.
- White blood cells, in particular, hold tremendous potential for gene therapists, as clever modifications can have profound impacts on cancer, autoimmunity, and viral infections.
With immense potential and practical advantages, it’s no surprise that CAR-T therapies are inducing remission in treatment-resistant cancers, CRISPR is altering fetal hemoglobin production to ameliorate sickle cell, and modified immune cells are challenging HIV without the same vulnerabilities as natural immune cells. By modifying HSCs, or stem-like T cell populations, altered daughter cells can continuously arise, navigate throughout the body, and correct the symptoms of disease by performing functions that diseased cells would otherwise fail to perform.
The versatility and accessibility of blood cells and their precursors provide a blank canvas for ingenuity. With the right creative thinking, these cells could serve as the foundation for a cure for cancer, inherited diseases, and infectious diseases. The technology is here, there is a precedent for this type of intervention, and there is an unmet medical need that demands our attention. The only limit is our creativity. For Jimi Olaghere, the future is here, and he is not the only one whose life can be changed using gene and cell therapy.
Here at Addimmune, we are on a mission to write the cure for HIV into reality. A growing list of blood disorders have been addressed using new gene therapy techniques, providing curative value to patients who would have otherwise needed lifelong care, and validating a suite of technologies which can be re-applied to our mission of creating a functional cure for HIV. As we look ahead to our future clinical trials, observing success in related gene therapy efforts and listening to the words of people like Jimi Olaghere gives us a glimpse of the future we are working to create. We know it’s possible, and for the millions of people living with HIV, we will continue working hard in pursuit of the missing cure.
